- Transdifferentiation in CF and COPD
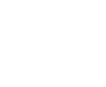
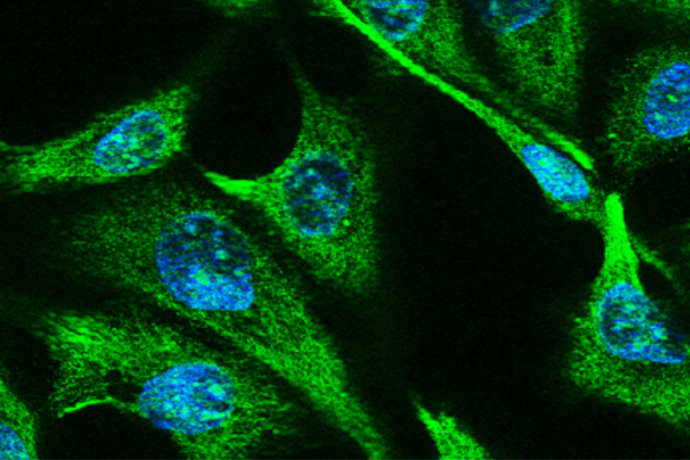
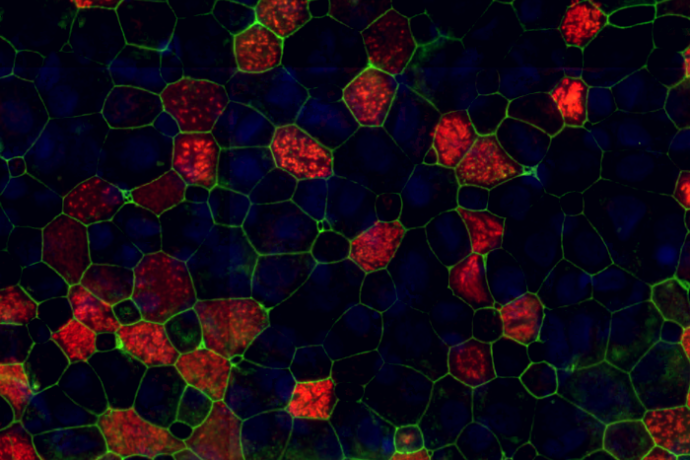
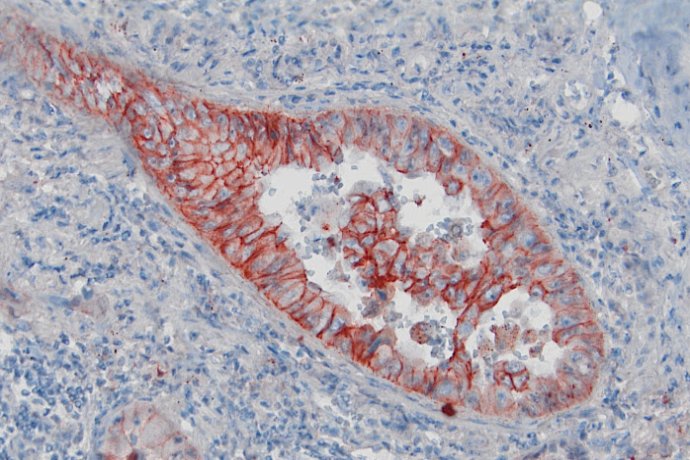
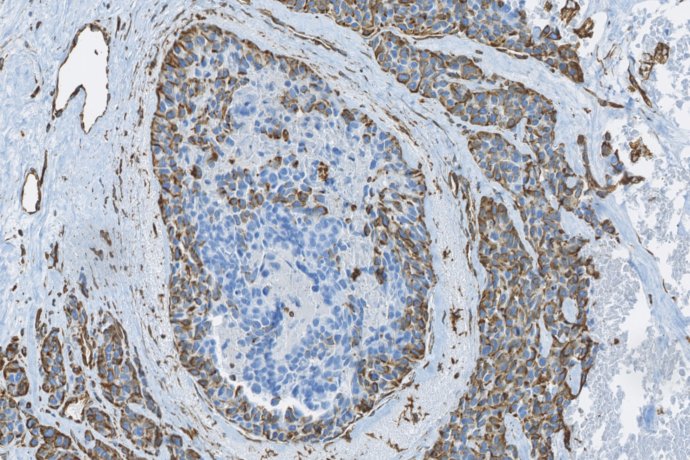
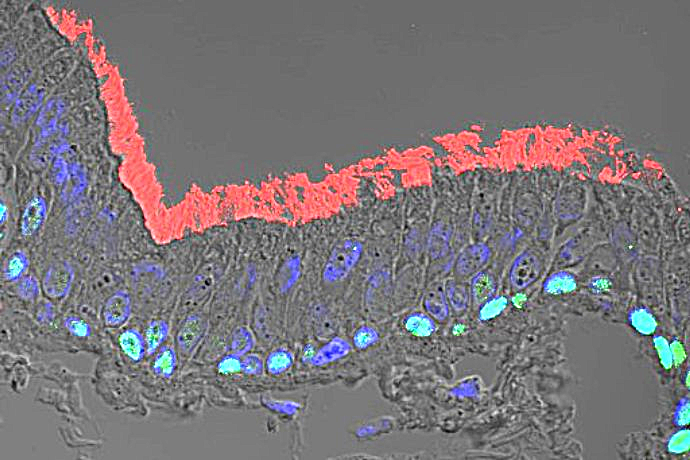
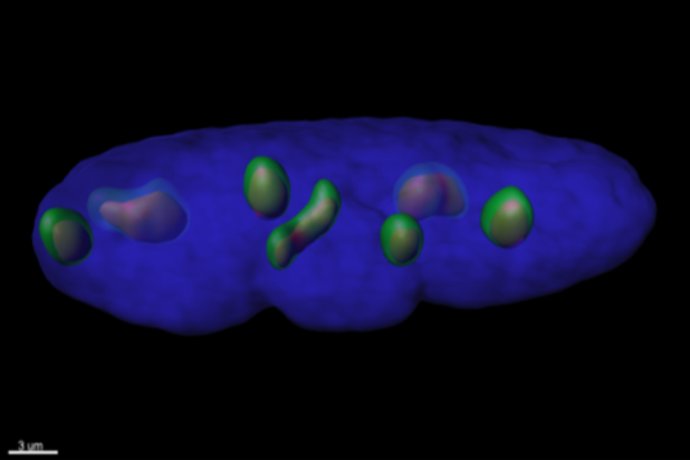
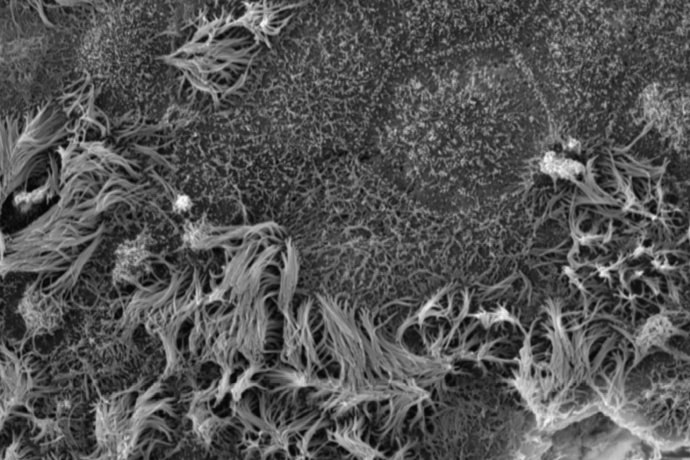
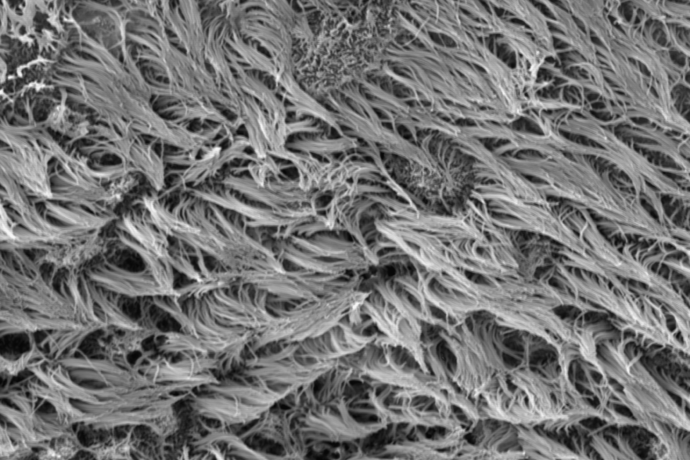
To study the mechanisms of regeneration and remodeling of the respiratory epithelium, we use primary respiratory cells dissociated from human endonasal or pulmonary surgical specimens from control subjects or patients with COPD and CF. Histological and immunohistochemical studies are performed in vivo, within the tissue of origin and in a mouse xenograft model; and in vitro in various three-dimensional culture models to analyze the expression of cell transdifferentiation markers. These in vitro culture models of respiratory cells in the air-liquid interface, either in the form of spheres in a liquid medium or a gel allow us to recapitulate the different stages of regeneration leading to the reconstitution of a mature and functional epithelium, but also to study the development of tissue remodeling. The factors involved in these phenomena as well as their impact on epithelial functionality, in terms of defense and mucociliary clearance, can thus be analyzed at the cellular and molecular levels. Moreover, these epithelial reconstitution approaches allow us to test the potential of pharmacological compounds for therapeutic purposes.
- Dedifferentiation and airway cancers
The study of dedifferentiation during tumor progression is addressed by in vivo and in vitro approaches. Histological and immunohistochemical analyses are performed on human specimens from the tumor bank of the Medical Biology and Pathology Department of the University Hospital of Reims and the Tumorotheque of Champagne-Ardenne. We also carry out functional studies from primary cultures and tumor cell lines using integrated molecular and cellular biology approaches. The cultured tumor cells are tested in in vitro models of invasion in the Boyden chamber, of 3D migration in collagen gel (dispersed cells or spheroids) coupled with image analysis systems developed in-house. This axis also resorts to in vivo mouse models reproducing the early and late stages of metastatic progression. These approaches allow to highlight new prognostic markers and to identify new anti-cancer therapeutic leads.
Although the mechanisms observed in these different pathologies are sometimes different, many molecules and physiopathological processes are involved in the plasticity of epithelial cells and are the subject of transversal work between the two themes of the Unit. Our research projects have shown that several factors could be considered biomarkers of airway remodeling. Our findings also demonstrated that these factors are functionally involved in the implementation of cellular plasticity in diverse lung pathologies, thus allowing us to suggest that they could be future therapeutic targets.